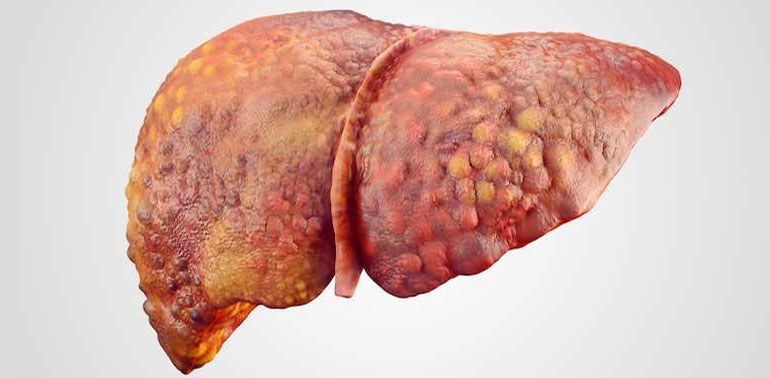
What is Liver Cirrhosis?
Liver cirrhosis is a progressive liver disease in which healthy liver tissue is replaced by scar tissue, impairing the liver’s ability to function properly. This scarring can result from various causes, such as chronic liver diseases, excessive alcohol consumption, or viral infections like hepatitis.
Over time, cirrhosis can lead to severe complications, including liver failure, liver cancer, and portal hypertension. Early detection and management are crucial to improving quality of life and slowing disease progression.
Causes of Liver Cirrhosis
Cirrhosis develops when the liver is repeatedly damaged and attempts to heal itself by forming scar tissue. Common causes include:
- Chronic Alcohol Abuse: Long-term heavy drinking is one of the most common causes of cirrhosis.
- Chronic Viral Hepatitis (B, C): Hepatitis B and C infections can lead to liver damage, cirrhosis, and even liver cancer over time.
- Fatty Liver Disease (NAFLD/NASH): Non-alcoholic fatty liver disease, often linked to obesity, diabetes, and metabolic syndrome, can progress to cirrhosis.
- Autoimmune Hepatitis: The body’s immune system mistakenly attacks liver cells, leading to inflammation and scarring.
- Inherited Liver Diseases: Genetic conditions like hemochromatosis (iron overload) or Wilson’s disease (copper buildup) can lead to cirrhosis.
- Bile Duct Diseases: Conditions such as primary biliary cholangitis (PBC) or primary sclerosing cholangitis (PSC) cause bile buildup and damage the liver.
Symptoms of Liver Cirrhosis
In the early stages, cirrhosis often has no symptoms. As the disease progresses, common signs and symptoms may include:
- Fatigue or weakness
- Jaundice (yellowing of the skin or eyes)
- Abdominal pain or discomfort (especially in the upper right side)
- Swelling in the abdomen (ascites) or legs
- Itchy skin
- Nausea or loss of appetite
- Easy bruising or bleeding
- Confusion or difficulty thinking clearly (hepatic encephalopathy)
- Dark urine and pale stools
Diagnosing Liver Cirrhosis
To diagnose cirrhosis, healthcare providers may use a combination of tests, including:
- Physical Examination: A doctor may look for signs of liver disease, such as an enlarged liver or spleen.
- Blood Tests: Liver function tests, including liver enzyme levels, can indicate liver damage or dysfunction.
- Imaging Tests: Ultrasound, CT scans, or MRI can assess liver size, shape, and the presence of scarring.
- Liver Biopsy: In some cases, a small sample of liver tissue is removed and examined to assess the extent of damage and scarring.
- Elastography (FibroScan): A non-invasive test that measures liver stiffness, often used to evaluate cirrhosis.
Stages of Cirrhosis
Cirrhosis progresses in stages:
- Stage 1 (Compensated Cirrhosis): The liver is damaged but still functions normally. Symptoms may be absent or mild.
- Stage 2 (Decompensated Cirrhosis): The liver begins to fail, and symptoms like jaundice, ascites, and encephalopathy may appear.
- Stage 3 (End-Stage Cirrhosis): Liver failure occurs, and serious complications like liver cancer or variceal bleeding can develop.
Treatment Options for Liver Cirrhosis
While cirrhosis cannot be cured, treatment focuses on managing the underlying cause, preventing further damage, and relieving symptoms. Treatment options include:
- Lifestyle Changes: Abstaining from alcohol, adopting a healthy diet, and managing comorbid conditions like diabetes and hypertension are essential.
- Medications: Antiviral drugs for hepatitis, diuretics for ascites, and lactulose for hepatic encephalopathy are common medications.
- Management of Complications: Treatment for varices, liver cancer, and ascites may include medications or procedures like endoscopic banding or paracentesis (fluid removal).
- Liver Transplantation: In cases of severe liver failure, a liver transplant may be considered.
Prevention of Liver Cirrhosis
While not all cases of cirrhosis can be prevented, certain lifestyle changes and precautions can reduce the risk:
- Limit Alcohol Consumption: Drink alcohol in moderation or avoid it altogether.
- Vaccination: Get vaccinated against hepatitis A and B to reduce the risk of liver infections.
- Manage Weight and Diet: Maintain a healthy weight, follow a balanced diet, and manage conditions like diabetes and high cholesterol.
- Avoid Hepatitis Transmission: Practice safe sex, avoid sharing needles, and ensure blood products are screened.
- Regular Health Check-ups: Routine blood tests and screenings for liver disease can help catch issues early, especially for people at high risk.
Living with Liver Cirrhosis
Living with cirrhosis requires ongoing care and management. Patients need to stay in close communication with their healthcare team to monitor liver function and adjust treatment plans as necessary. It’s important to manage symptoms and prevent complications by making healthy lifestyle choices, adhering to treatment regimens, and attending regular check-ups.
When to Seek Medical Attention
If you experience any of the following signs or symptoms, seek medical attention immediately:
- Sudden, severe abdominal pain
- Uncontrollable bleeding or bruising
- Worsening confusion or difficulty thinking
- Swelling in the abdomen or legs
- Signs of infection, such as fever or chills
 Get Clinic or Online Consultation
Get Clinic or Online Consultation