What is Pancreatitis?
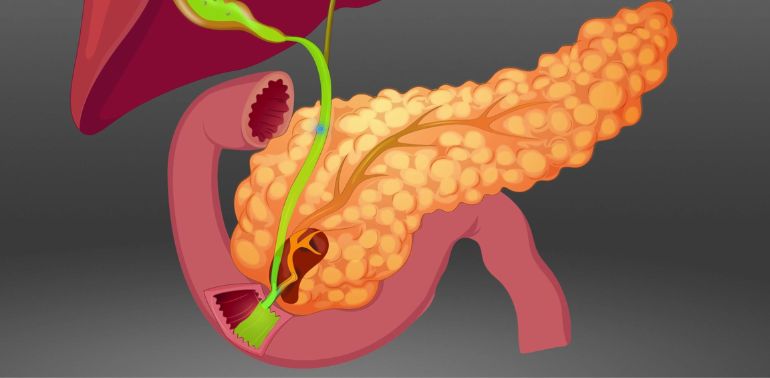
Pancreatitis is the inflammation of the pancreas, a vital organ located behind your stomach. The pancreas plays a key role in digestion by producing digestive enzymes and hormones, such as insulin, which regulates blood sugar levels. When the pancreas becomes inflamed, it can cause symptoms ranging from mild discomfort to severe pain and life-threatening complications.
There are two main types of pancreatitis:
Acute Pancreatitis: This is a sudden inflammation of the pancreas that lasts for a short time. It can develop quickly and is often severe, but with prompt treatment, most people recover fully.
Chronic Pancreatitis: This is a long-term condition where the pancreas becomes permanently damaged over time, leading to ongoing inflammation. It can result in complications such as pancreatic insufficiency (where the pancreas does not produce enough enzymes or hormones), diabetes, or pancreatic cancer.
What Causes Pancreatitis?
The causes of pancreatitis can vary, but the most common factors include:
Gallstones: These small, hard deposits can block the bile duct and the pancreatic duct, leading to inflammation in the pancreas. This is the leading cause of acute pancreatitis.
Excessive Alcohol Consumption: Chronic heavy drinking is a major risk factor for both acute and chronic pancreatitis. Alcohol can irritate the pancreas and lead to long-term damage.
High Blood Triglyceride Levels: Elevated levels of triglycerides (a type of fat in the blood) can cause acute pancreatitis, especially when levels exceed 1,000 mg/dL.
Medications: Certain medications, including steroids, diuretics, and some antibiotics, can trigger pancreatitis as a side effect.
Trauma or Surgery: Injury to the abdomen or gallbladder surgery can damage the pancreas and cause inflammation.
Infections: Viral infections, such as mumps or hepatitis, can lead to pancreatitis, although this is less common.
Genetic Factors: In some cases, pancreatitis can be inherited, with genetic mutations causing a higher risk of developing the condition.
Other Factors: Conditions such as high blood calcium levels, cystic fibrosis, pancreatic duct abnormalities, or autoimmune disorders can also lead to pancreatitis.
Symptoms of Pancreatitis
The symptoms of pancreatitis can vary depending on whether it is acute or chronic:
Acute Pancreatitis
Symptoms typically appear suddenly and may include:
- Severe abdominal pain, typically in the upper abdomen, which may radiate to the back.
- Nausea and vomiting.
- Fever and chills.
- Rapid pulse or increased heart rate.
- Swollen or tender abdomen.
- Jaundice (yellowing of the skin or eyes), especially if the bile duct is obstructed.
- Unexplained weight loss.
Chronic Pancreatitis
Symptoms may develop over time and include:
- Persistent or recurrent abdominal pain, often after eating.
- Nausea and vomiting, especially after large or fatty meals.
- Fatty stools (steatorrhea) that are greasy, foul-smelling, and difficult to flush.
- Unexplained weight loss due to malabsorption of nutrients.
- Jaundice.
- Signs of diabetes, such as increased thirst or frequent urination, if insulin production is affected.
Diagnosis of Pancreatitis
If your doctor suspects pancreatitis, they will perform a thorough evaluation that may include:
Physical Examination: The doctor will examine your abdomen for tenderness or swelling, and assess for signs of jaundice.
Blood Tests: Blood tests are commonly used to diagnose pancreatitis. Elevated levels of amylase and lipase (enzymes produced by the pancreas) are key indicators of inflammation in the pancreas.
Imaging Tests: Imaging studies, such as an ultrasound, CT scan, or MRI, may be used to check for gallstones, pancreatic swelling, or other complications.
Endoscopic Procedures: If a blockage in the pancreatic or bile ducts is suspected, your doctor may recommend an endoscopic ultrasound or endoscopic retrograde cholangiopancreatography (ERCP), which allows for a detailed view of the pancreas and bile ducts and may help to remove stones or blockages.
Pancreatic Function Tests: In cases of chronic pancreatitis, tests that assess the ability of the pancreas to produce enzymes and hormones may be used.
Treatment Options for Pancreatitis
Treatment for pancreatitis depends on the severity of the condition and whether it is acute or chronic. In both cases, the main goals of treatment are to relieve pain, reduce inflammation, and address the underlying cause of the condition.
Acute Pancreatitis Treatment
Hospitalization: Most people with acute pancreatitis need to be admitted to the hospital for treatment and monitoring. This is especially important if the condition is severe.
Fasting: Patients may need to avoid eating or drinking for a period of time to allow the pancreas to heal and reduce inflammation.
Pain Management: Medications to manage pain, such as acetaminophen or opioids, may be used depending on the severity of the pain.
Intravenous (IV) Fluids: Dehydration is common in pancreatitis, and IV fluids are administered to maintain hydration and support normal body functions.
Treating Underlying Conditions: If gallstones, high triglycerides, or alcohol use is the cause, the doctor may recommend specific treatments, such as gallbladder removal, triglyceride-lowering medications, or counseling and support for alcohol cessation.
Surgical Interventions: In cases where there are complications such as pancreatic abscesses, infected tissue, or blockages in the bile or pancreatic ducts, surgery may be required to remove damaged tissue or stones.
Chronic Pancreatitis Treatment
Lifestyle Changes: Avoiding alcohol and eating a low-fat, balanced diet are essential for managing chronic pancreatitis. Smoking cessation is also strongly recommended, as smoking can worsen the condition.
Pain Management: Chronic pancreatitis often causes ongoing pain, which may require medications such as pain relievers or specific drugs for nerve pain.
Enzyme Replacement Therapy: As the pancreas becomes less able to produce digestive enzymes, enzyme replacement therapy may be prescribed to help the body digest food properly.
Managing Diabetes: If chronic pancreatitis leads to diabetes, patients may require insulin or oral medications to manage blood sugar levels.
Surgical Interventions: In some cases, surgery may be needed to remove damaged parts of the pancreas, drain fluid collections, or relieve blockages. Pancreatic surgery may include pancreaticojejunostomy or pancreatic resection.
When to Seek Medical Attention
If you experience any of the following symptoms, seek immediate medical attention:
- Severe abdominal pain that comes on suddenly and worsens over time.
- Fever, chills, and vomiting.
- Yellowing of the skin or eyes (jaundice).
- Difficulty breathing or feeling faint.
- Severe nausea and vomiting that prevents you from keeping food or fluids down.
These could indicate complications from pancreatitis, such as pancreatic necrosis (tissue death), infection, or pancreatic pseudocyst.
Complications of Pancreatitis
If left untreated or if severe, pancreatitis can lead to serious complications, including:
- Pancreatic Necrosis: Death of pancreatic tissue that can lead to infection and widespread inflammation.
- Pancreatic Pseudocysts: Fluid-filled sacs that can form on the pancreas and lead to infection or rupture.
- Diabetes: Chronic pancreatitis can damage the insulin-producing cells of the pancreas, leading to diabetes.
- Malabsorption: Damage to the pancreas can impair its ability to secrete digestive enzymes, resulting in difficulty digesting food and nutrient deficiencies.
- Pancreatic Cancer: Chronic inflammation of the pancreas may increase the risk of developing pancreatic cancer.
Prevention of Pancreatitis
While not all cases of pancreatitis can be prevented, certain lifestyle changes can help reduce your risk:
- Avoid excessive alcohol consumption.
- Maintain a healthy weight and manage your cholesterol levels.
- Eat a balanced, low-fat diet rich in fruits, vegetables, and whole grains.
- Exercise regularly to maintain overall health.
- Monitor your blood triglyceride levels, especially if you have a history of high cholesterol or heart disease.
 Get Clinic or Online Consultation
Get Clinic or Online Consultation