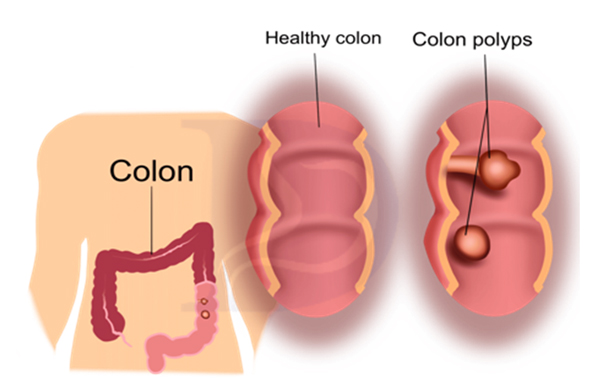
A colon polyp is a growth on the inner lining of the colon (large intestine) or rectum. Polyps in the colon arise from uncontrolled multiplication of cells leading to growth of tissue. This can occur due to mutation in the genes of the
cells. A polyp can vary in size from few millimeters to several centimeters. Polyps look like mushrooms and can have a variety of shapes. They can be flat, slightly raised, or have a stalk.
COLON POLYS AND COLON CANCER
What are colon polyps and why should you look for them?
What are colon polyps?
What are the types of colon polyps?
Essentially there are two types of polyps. “Hyperplastic polyps” which are not pre-cancerous and “Adenomatous polyps or adenomas” which are pre-cancerous. The type of the polyp can be determined only after its removal.
How do colon polyps progress to colon cancer?
Pre-cancerous polyps (adenomas) may continue to grow in size, develop into cancer and invade surrounding tissues. It takes approximately 10 years for a small polyp to develop into cancer. Only 5-10% of all polyps will progress to cancer. Polyps larger than 1 cm are more likely to become cancer.
Who is at risk of developing colon polyps?
Polyps are found in about 30% of the adult population over the age of 45. Men and women of all ethnicities are at risk of developing colon polyps.
Many factors including diet, lifestyle, older age, and genetics increases the risk for polyps. Important factors predisposing to colon polyps and cancer include:
• Smoking
• Excess alcohol consumption
• Lack of exercise
• Obesity
• Eating processed foods and too much red meat
• Family history of colon polyps or cancer
• Personal history of inflammatory bowel disease
How common is colon cancer?
Colon cancer is the third most common cancer worldwide. Almost 2 million cases are diagnosed every year. It is the second most common cause of death due to cancer, leading to almost 1 million deaths every year. It is estimated that the incidence of colon cancer will increase by almost 50% in the next 20 years. Most of this increase is expected to occur in countries transitioning to the developed world and this includes large parts of Asia and Middle East.
What are the symptoms of colon polyps?
Most colon polyps and early colorectal cancer do not have any symptoms, which is why screening is recommended. However, when symptoms do occur, they may include:
• Blood in the stools
• Unexplained anemia or weight loss.
• Change in normal bowel movement pattern.
What is colon cancer screening?
Ninety percent of all colon cancers start as polyps.
Therefore, the best way to prevent colon cancer is to look for precancerous polyps inside the colon and remove them before they progress to cancer.
How is screening done for colon cancer?
Screening involves direct visualization of the inner lining of the colon to detect polyps. This can be done either by colonoscopy or sigmoidoscopy. Non-invasive techniques such as virtual colonoscopy using a CT scan or image capture by a ingestible capsule camera can also visualize the colon lining. Other colon cancer screening tests involve stool analysis for presence of occult blood which may indirectly suggest the presence of colon polyps. It is recommended to start screening at the age of 45.
What is screening colonoscopy?
While a colonoscopy takes a thorough look at the whole of the colon, a sigmoidoscopy examines the rectum and the lower third of the colon. Since 80% of all precancerous polyps are found in the rectum and lower third of the colon, a sigmoidoscopy is a good alternative to colonoscopy for cancer screening. A sigmoidoscopy does not require elaborate bowel cleansing and can be performed without sedation hence making the procedure brief and easier. For those opting for sigmoidoscopy, it should be done once every 5 years and should ideally be combined with the annual stool occult blood test.
What is a sigmoidoscopy?
While a colonoscopy takes a thorough look at the whole of the colon, a sigmoidoscopy examines the rectum and the lower third of the colon. Since 80% of all precancerous polyps are found in the rectum and lower third of the colon, a sigmoidoscopy is a good alternative to colonoscopy for cancer screening. A sigmoidoscopy does not require elaborate bowel cleansing and can be performed without sedation hence making the procedure brief and easier. For those opting for sigmoidoscopy, it should be done once every 5 years and should ideally be combined with the annual stool occult blood test.
What is virtual colonoscopy?
Virtual colonoscopy, also known as CT colonography uses a CT scan to gather cross-sectional images of your abdomen followed by 3-D reconstruction of the colon. It can detect polyps larger than 5 mm. It is less invasive than a traditional colonoscopy. Bowel cleansing is required but sedation is not needed.
However, once a polyp is detected, a colonoscopy is needed to remove the polyp. A virtual colonoscopy is recommended once in 5 years for colon cancer screening.
What is the stool occult blood test?
Polyps and colorectal cancers often bleed a small amount, and this blood may not be visible to the naked eye. The stool occult blood test, also known as the faecal immunochemical test (FIT) detects tiny amounts of blood in stool samples. A positive stool occult blood test does not always mean presence of a polyp or cancer. Ulcers, inflammation in the gut and even haemorrhoids (piles) can cause a positive test result. A stool occult blood test is recommended once a year after the age of 45 years. A colonoscopy is recommended in case of a positive test.
What is the stool DNA test?
Cells from polyps and cancers are shed in the stool. A special stool test looks for mutations in the DNA of these cells. The stool DNA test targets multiple DNA markers to achieve high detection rates. These DNA markers are present in only trace quantities in the stool and therefore highly sensitive laboratory methods are used to detect these markers. The stool DNA test has been demonstrated to have high detection rates for early-stage colon cancer. This test is recommended once every two years. A colonoscopy is recommended in case of a positive test.
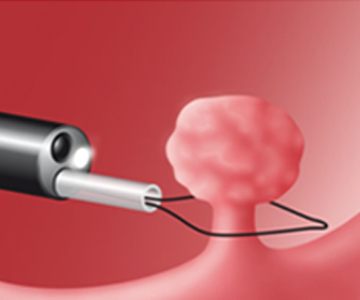
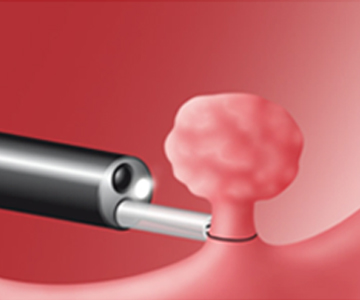
How are colon polyps removed?
Polyps can be easily removed during colonoscopy or sigmoidoscopy using a technique called snare polypectomy. Larger and complex polyps require advanced techniques such as endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD).

What happens after a colon polyp is removed?
After a polyp is removed during colonoscopy, it is subjected to pathological analysis to determine if it is a precancerous polyp (adenoma) or a non-cancerous polyp (hyperplastic). Individuals who have adenomas on an initial colonoscopy are at a higher risk of developing more adenomas and cancers and therefore require more frequent colonoscopies (once every 3-5 years) depending upon the number and size of the polyps.
What is the significance of family history of colon polyps and colon cancer?
A family history of colon cancer means that you have an immediate family member (or multiple other family members) who have had colon cancer. As many as 1 in 3 people who develop colorectal cancer have a family history of colon polyps or colorectal cancer. For those with a strong family history, a colonoscopy should be repeated at least every five years. Colonoscopy screening should begin at 40 years or 10 years earlier than the earliest case of colon cancer in the family.

How can artificial intelligence (AI) help in detection of colon polyps?
Artificial intelligence software programs are now being used during colonoscopy to pick up very small polyps (<5 mm) that may be missed on routine visual examination. Use of AI, therefore, increases polyp detection during colonoscopy. Newer AI programs can also predict the type of polyp (hyperplastic vs. adenoma) without need for a biopsy. Use of AI may therefore soon become the standard of care during screening colonoscopy.
What is a colon capsule?
A colon capsule is a small electronic device that contains a high-resolution camera and a light source. The colon capsule is swallowed and passes through the entire gut to reach the colon. It is designed to take thousands of pictures of the colon. These pictures are transmitted to an external wearable device and can be analyzed later by the physician often with the help of AI programs. While colon capsule is still not a recommended test for detection of colon polyps and cancer, the technology is non-invasive and quite appealing as a screening test once it is validated in clinical trials.
How can colon cancer be prevented?
It is possible to reduce the risk of colon cancer by lifestyle modifications. These include:
• Avoiding excess alcohol.
• Quitting smoking and tobacco.
• Losing any extra weight to normalize your BMI.
• Regular exercise, about 30 minutes a day.
• Having 3-5 servings of fruits & vegetables daily.
• Avoiding fatty foods, processed foods and red meat in excess.
• Considering screening for colon polyps by one of the standard screening methods starting at the age of 45 years
STANDARD TESTS FOR COLORECTAL CANCER SCREENING
(Recommended starting age 45)

If you have any questions please fell free to contact with us.
